Sepsis cannot be addressed by a single medical discipline, or by targeting only the biomedical community.
Preventing and mitigating its burden is not possible without addressing related social determinants, including underlying malnutrition and access to care. Action on Sepsis is well positioned to leverage the incredible pool of experts throughout UBC to address sepsis through three main research directions.
- Facilitating adoption of infection prevention and control (IPC) programs. Focusing on prevention is important to reducing the burden of sepsis globally, since the costs of managing sepsis increase with increasing severity of the syndrome. In BC, preventing just 1,153 people from acquiring sepsis from 2014-2018 was estimated to contribute to $51M of savings from reduced in-hospital and follow-up care and out of-pocket burial costs. IPC occupies a unique position in improving safety and quality of care for sepsis, as it is universally relevant to every health worker and patient. Yet a global survey carried out by the WHO in 2021-2022 found that only 4 out of 106 countries had all minimal requirements for national IPC programs. We seek to address this gap by advocating for and supporting the implementation and evaluation of comprehensive IPC programs , focusing on low-resource contexts where the gains are likely to be immense.
-
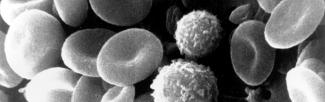
Catalyzing discovery science for pandemic preparedness. During a pandemic, most deaths from severe infections are from sepsis. Improved sepsis-related diagnostics and therapeutics will be critical in future pandemic responses. Thus, increasing our understanding of the biology of sepsis and integrating these insights into clinical practice must be a cornerstone of pandemic preparedness and response. During the COVID-19 pandemic, our members developed pan-Canadian and international clinical networks to facilitate data sharing and rapid knowledge exchange, led innovation in vaccines, diagnostics, and therapeutics [4,6], and advocated for increased recognition of the long-term impacts of severe infectious diseases. Our cluster will leverage this momentum to develop, evaluate, and commercialize new vaccines, diagnostics, and therapies. We seek to scale data-driven approaches that leverage clinical risk prediction to help health workers identify those who are most vulnerable and guide delivery of care, and validate and commercialize approaches to managing sepsis that are guided by an individual’s gene expression signature and clinical presentation.
-
Building health literacy through knowledge exchange with non-academic partners. Globally, public awareness of sepsis is low. In a recent survey, 39% of Canadians had not heard of sepsis, and only 32% knew about signs, risk factors, and strategies to lower risk. Yet sepsis can be prevented by simple means (e.g., vaccines, hand hygiene), and early recognition of suspected sepsis is crucial: every hour of delay in treatment is associated with an increase in the risk of disability and death. Simple and persuasive public education messages can promote healthy practices and encourage timely care-seeking for suspected sepsis. We aim to catalyze new collaborations between health workers, policy-makers, industry, advocacy partners (e.g., BC Patient Safety & Quality Council, Global Sepsis Alliance, Canadian Sepsis Foundation) and UBC researchers with expertise in infectious diseases, health promotion, and community engagement, in order to develop and disseminate these messages and evaluate the impact of our knowledge mobilization strategies.